The Ketogenic Diet Reverses Indicators of Heart Disease
Cardiovascular disease (CVD) is the leading cause of death worldwide
[1]. Because of its prevalence and life-threatening nature, and because it appears that a keto diet is likely to reverse it, we consider it one of the most important conditions to discuss here.
In our last post, we argued that CVD, being a disease strongly associated with metabolic syndrome, is likely to be best treated with a ketogenic diet. In this post we will present more evidence that ketogenic diets do improve heart disease risk factors.
Unfortunately, there is much confusion and misinformation about the impact of nutrition on CVD among scientists and non-scientists alike. Not only does a high fat, keto diet not worsen heart disease risk — as would commonly be assumed — it actually improves it. This confusion about dietary fat is probably the reason that we do not yet have clinical trials directly testing the effects of ketogenic diets on CVD outcomes.
However, we already have many trials of ketogenic diets that measured known CVD risk factors, especially cholesterol profiles. It turns out that these trials show a powerful heart disease risk reduction in those following a ketogenic diet. It is powerful both in absolute terms, and in comparison with low-fat diets, which tend to improve some weakly predictive factors while worsening stronger predictors.
As such, a high-fat ketogenic diet is currently the best known non-drug intervention for heart disease, as defined by mainstream measures of risk. It is arguably better than drug interventions, too.
In brief:
- Total cholesterol and LDL cholesterol are only weak predictors of CVD.
- Triglycerides, HDL, LDL particle size, and the HDL-to-triglyceride ratio are much stronger predictors of CVD.
- Keto diets improve triglyceride levels, HDL, and LDL particle size — precisely those measures that strongly indicate risk.
Total cholesterol and LDL cholesterol are only weakly associated with CVD
The connection between blood cholesterol levels and the development of heart disease began to be explored in the last century. Over the last several decades, our understanding of the predictive power of various blood lipids has gone through many refinements as our ability to measure finer and finer detail has advanced.
In the early years, it appeared that high levels of total cholesterol carried some risk of heart disease in many cases. However, it is now well established that total cholesterol by itself is a weak predictor [2, 3, 4].
The reason is quite simple. The different subtypes of cholesterol work together in an intricately balanced system. There is a wide range of total cholesterol levels that are perfectly healthy, so long as the proportions of the subtypes are healthy ones. By the same token, a given level of total cholesterol, even if it is perfectly normal, could be pathological when examined by subtype. Strong evidence from recent decades suggests that the best known blood lipid measures for predicting future risk of CVD are HDL, triglycerides, and related ratios (see below).
Similarly, while LDL cholesterol is probably important, it appears that it does not have good predictive power when looking at its magnitude alone [5, 6, 7, 8].
One reason for this is that like total cholesterol, LDL is not uniform. Just as we distinguish between HDL and LDL, the so-called “good” and “bad” cholesterol, LDL itself is now known to have two important subtypes with opposite risk implications. Having more large, light LDL particles (also called Pattern A), does not indicate high CVD risk, but having more small, dense particles (Pattern B) does [9, 10, 11, 12, 13]. Therefore high LDL by itself is not necessarily indicative of CVD.
Low HDL cholesterol is strongly associated with CVD
Having high blood levels of HDL is now widely recognized as predicting lower levels of heart disease. The proportion of total cholesterol that is HDL cholesterol is a particularly strong predictor. In 2007, a meta-analysis was published in the Lancet that examined information from 61 prospective observational studies, consisting of almost 900,000 adults. Information about HDL was available for about 150,000 of them, among whom there were 5000 vascular deaths. According to the authors, “the ratio of total to HDL cholesterol is a substantially more informative predictor of IHD mortality than are total cholesterol, HDL cholesterol, or non-HDL cholesterol.” [14]
This is consistent with many other studies, for example this very recent analysis from the COURAGE trial [15].
High triglycerides are strongly associated with CVD
There has been drawn out controversy in the medical community as to the relationship of triglyceride levels to CVD. There are two parts to the controversy: whether or not triglycerides are an independent predictor of CVD, and whether or not triglycerides play a causative role in CVD.
In both cases, however, it doesn’t matter in which way the controversy is resolved! Whether or not triglycerides independently predict CVD (and there is at least some evidence that they do), and whether or not they cause CVD, there is no controversy about whether they predict CVD. The association between triglyceride levels and CVD still holds and is strongly predictive [16, 17, 18]. In fact it is so predictive that those who argue that triglyceride levels are not an independent risk factor, call it instead a “biomarker” for CVD [19]. In other words, seeing high triglycerides is tantamount to seeing the progression of heart disease.
HDL-to-Triglycerides Ratio: compounding evidence
Triglycerides and HDL levels statistically interact. That means it is a mistake to treat one as redundant with respect to the other. If you do, you will miss the fact that the effect of one on your outcome of interest changes depending on the value of the other. Despite the fact that most heart disease researchers who study risk factors have not used methods tuned to find interactions between triglycerides and HDL, many studies have at least measured both. This has allowed others to do the appropriate analysis. When triglycerides and HDL have been examined with respect to each other, that is, when the effect of triglycerides is measured under the condition of low HDL, or when the effect of HDL is measured under the condition of high triglycerides, this combination of factors turns out to be even more indicative of CVD [20, 21, 22, 23].
One of the most interesting aspects of this finding from our perspective, is that the ratio of triglyceride levels to HDL is considered to be a surrogate marker of insulin resistance (See The Ketogenic Diet as a Treatment for Metabolic Syndrome.) In other words, the best lipid predictors of CVD are also those that indicate insulin resistance.
Ketogenic Diets improve risk factors for CVD
There is now ample evidence that a low carbohydrate, ketogenic diet improves lipid profiles, particularly with respect to the risk factors outlined above: triglycerides, HDL, and their ratio [24, 25, 26, 27, 28, 29, 30, 31].
Although a ketogenic diet typically raises LDL levels, which has been traditionally seen as a risk factor, it has also been shown to improve LDL particle size. In other words, although the absolute amount of LDL goes up, it is the “good” LDL that goes up, whereas the “bad” LDL goes down [31, 32]. This is hardly surprising, since LDL particle size is also strongly predicted by triglycerides [33, 34, 35].
Although there have not yet been intervention studies testing the effect of a ketogenic diet on the rate of actual CVD incidents (e.g. heart attacks), the evidence about lipid profiles is strong enough to make ketogenic diets more likely to reduce heart disease than any other known intervention.
Summary:
- Current medical practice uses blood lipid measurements to assess the risk of heart disease.
- Despite the continuing tradition of measuring total cholesterol and LDL, we have known for decades that triglycerides, HDL, and the ratio of the two, are much better predictors of heart disease. LDL particle size is also considered strongly predictive.
- A ketogenic diet has a very favourable impact on these risk factors, and thus should be considered the diet of choice for those at risk of CVD.
In their 2011 paper, “Low-carbohydrate diet review: shifting the paradigm”, Hite et al. display the following graph (VLCKD stands for Very Low Carbohydrate Ketogenic Diet, and LFD for Low Fat Diet) [36] based on data from [31]:
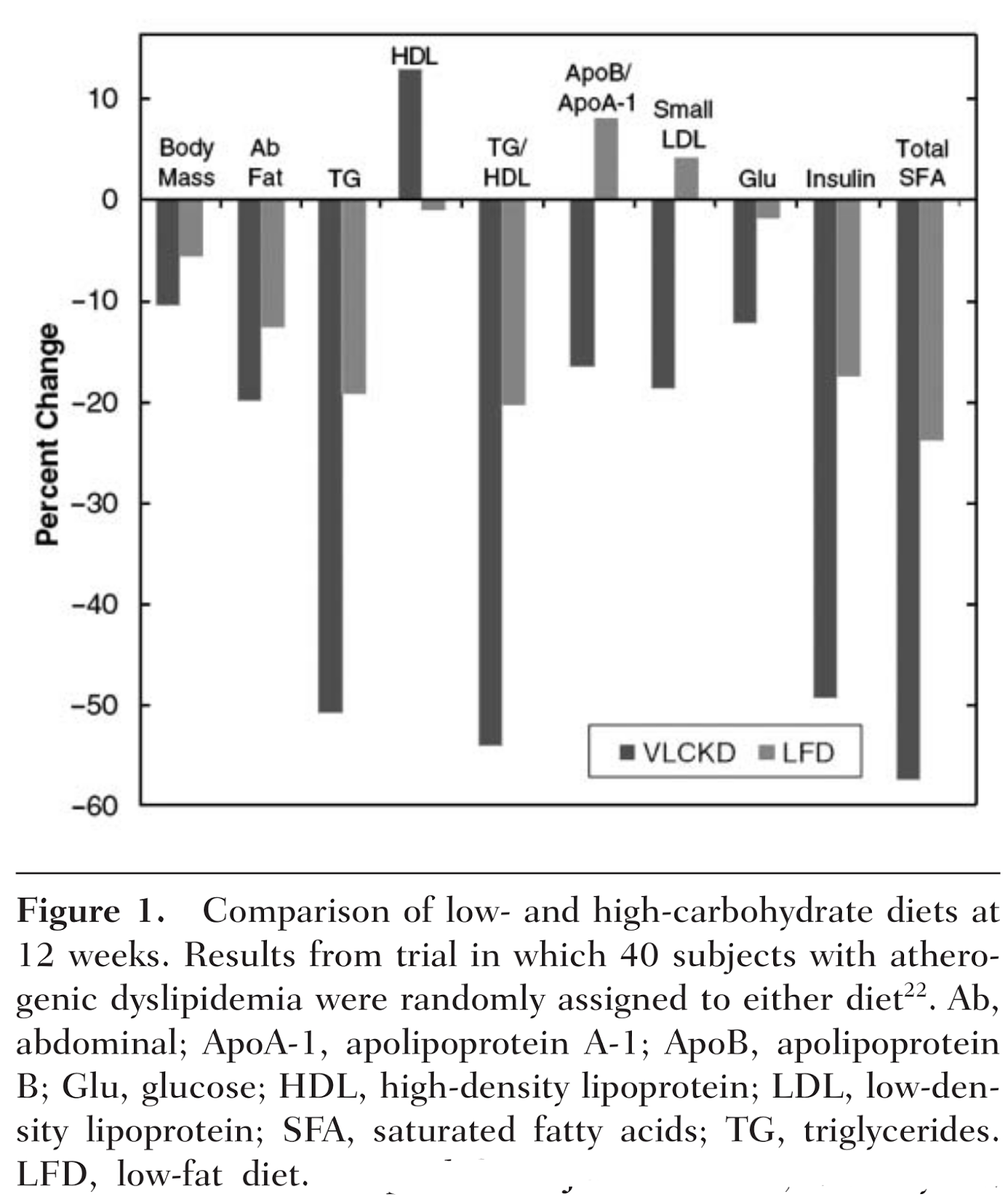
It makes an excellent visualization of the factors at stake, and how powerful a ketogenic diet is. It also shows quite clearly that not only is restricting carbohydrate more effective for this purpose than a low fat diet, but that a low fat diet is detrimental for some important risk factors — apolipoprotein ratios, LDL particle size, and HDL — but a low carb diet is not. The ketogenic diet resulted in a significant improvement in every measure.
References:
1. Evidence type: observational
World Health Organization Fact sheet N°317: Cardiovascular diseases (CVDs) September 2011
- CVDs are the number one cause of death globally: more people die annually from CVDs than from any other cause.
- An estimated 17.3 million people died from CVDs in 2008, representing 30% of all global deaths. Of these deaths, an estimated 7.3 million were due to coronary heart disease and 6.2 million were due to stroke.
- Low- and middle-income countries are disproportionally affected: over 80% of CVD deaths take place in low- and middle-income countries and occur almost equally in men and women.
- By 2030, almost 23.6 million people will die from CVDs, mainly from heart disease and stroke. These are projected to remain the single leading causes of death.
2. Evidence type: observational
Role of lipid and lipoprotein profiles in risk assessment and therapy.
Ballantyne CM, Hoogeveen RC. Am Heart J.
2003 Aug;146(2):227-33.
Despite a strong and consistent association within populations, elevated TC [(total cholesterol)] alone is not a useful test to discriminate between individuals who will have CHD [(coronary heart disease)] events and those who will not.
3. Evidence type: observational
Relation of serum lipoprotein cholesterol levels to presence and severity of angiographic coronary artery disease.
Philip A. Romm, MD, Curtis E. Green, MD, Kathleen Reagan, MD, Charles E. Rackley, MD.
The American Journal of Cardiology Volume 67, Issue 6, 1 March 1991, Pages 479–483
Most CAD [(coronary artery disease)] occurs in persons who have only mild or moderate elevations in cholesterol levels. Total cholesterol level alone is a poor predictor of CAD, particularly in older patients in whom the major lipid risk factor is the HDL cholesterol level.
4. Evidence type: observational
Lipids, risk factors and ischaemic heart disease.
Atherosclerosis. 1996 Jul;124 Suppl:S1-9.
Castelli WP.
Those individuals who had TC [(total cholesterol)] levels of 150-300 mg/dl (3.9-7.8 mmol/1) fell into the overlapping area (Fig. 1), demonstrating that 90% of the TC levels measured were useless (by themselves) for predicting risk of CHD [(coronary heart disease)] in a general population. Indeed, twice as many individuals who had a lifetime TC level of less than 200 mg/dl (5.2 mmol/1) had CHD compared with those who had a TC level greater than 300 mg/dl (7.8 mmol/l) (Fig. 1).
5. Evidence type: observational
Range of Serum Cholesterol Values in the Population Developing Coronary Artery Disease.
William B. Kannel, MD, MPH.
The American Journal of Cardiology, Volume 76, Issue 9, Supplement 1, 28 September 1995, Pages 69C–77C
The ranges of serum cholesterol and LDL cholesterol levels varied widely both in the general population and in patients who had already manifested CAD (Figures 1 and 2). Because of the extensive overlap between levels, it was impossible to differentiate the patients with CAD from the control subjects.
6. Evidence type: observational
Lipoprotein cholesterol, apolipoprotein A-I and B and lipoprotein (a) abnormalities in men with premature coronary artery disease.
Jacques Genest Jr., MD,FACC, Judith R. McNamara, MT, Jose M. Ordovas, PhD, Jennifer L. Jenner, BSc, Steven R. Silberman, PhD, Keaven M. Anderson, PhD, Peter W.F. Wilson, MD, Deeb N. Salem, MD, FACC, Ernst J. Schaefer, MD.
Journal of the American College of Cardiology Volume 19, Issue 4, 15 March 1992, Pages 792–802.
Our data suggest that total and LDL cholesterol may not be the best discriminants for the presence of coronary artery disease despite the strong association between elevated cholesterol and the development of coronary artery disease in cross-sectional population studies and prospective epidemiologic studies.
7. Evidence type: observational
Apolipoprotein B and apolipoprotein A-I: risk indicators of coronary heart disease and targets for lipid-modifying therapy.
Walldius, G. and Jungner, I. (2004),
Journal of Internal Medicine, 255: 188–205. doi: 10.1046/j.1365-2796.2003.01276.x
(Emphasis ours.)
For over three decades it has been recognized that a high level of total blood cholesterol, particularly in the form of LDL cholesterol (LDL-C), is a major risk factor for developing coronary heart disease (CHD) [1–4]. However, as more recent research has expanded our understanding of lipoprotein function and metabolism, it has become apparent that LDL-C is not the only lipoprotein species involved in atherogenesis. A considerable proportion of patients with atherosclerotic disease have levels of LDL-C and total cholesterol (TC) within the recommended range [5, 6], and some patients who achieve significant LDL-C reduction with lipid-lowering therapy still develop CHD [7].
Other lipid parameters are also associated with elevated cardiovascular risk, and it has been suggested that LDL-C and TC may not be the best discriminants for the presence of coronary artery disease (CAD) [5].
8. Evidence type: observational
Plasma Lipoprotein Levels as Predictors of Cardiovascular Death in Women.
Katherine Miller Bass, MD, MHS; Craig J. Newschaffer, MS; Michael J. Klag, MD, MPH; Trudy L. Bush, PhD, MHS.
Arch Intern Med. 1993;153(19):2209-2216.
Using a sample of 1405 women aged 50 to 69 years from the Lipid Research Clinics’ Follow-up Study, age-adjusted CVD death rates and summary relative risk (RR) estimates by categories of lipid and lipoprotein levels were calculated. Multivariate analysis was performed to provide RR estimates adjusted for other CVD risk factors.
RESULTS: Average follow-up was 14 years. High-density lipoprotein and triglyceride levels were strong predictors of CVD death in age-adjusted and multivariate analyses. Low-density lipoprotein and total cholesterol levels were poorer predictors of CVD mortality. After adjustment for other CVD risk factors, HDL levels less than 1.30 mmol/L (50 mg/dL) were strongly associated with cardiovascular mortality (RR = 1.74; 95% confidence interval [CI], 1.10 to 2.75). Triglyceride levels were associated with increased CVD mortality at levels of 2.25 to 4.49 mmol/L (200 to 399 mg/dL) (RR = 1.65; 95% CI, 0.99 to 2.77) and 4.50 mmol/L (400 mg/dL) or greater (RR = 3.44; 95% CI, 1.65 to 7.20). At total cholesterol levels of 5.20 mmol/L (200 mg/dL) or greater and at all levels of LDL and triglycerides, women with HDL levels of less than 1.30 mmol/L (< 50 mg/dL) had CVD death rates that were higher than those of women with HDL levels of 1.30 mmol/L (50 mg/dL) or greater.
9. Evidence type: plausible mechanism and observational review
Particle size: the key to the atherogenic lipoprotein?
Rajman I, Maxwell S, Cramb R, Kendall M.
QJM. 1994 Dec;87(12):709-20.
Using different analytical methods, up to 12 low-density lipoprotein (LDL) subfractions can be separated. LDL particle size decreases with increasing density. Smaller, denser LDL particles seem more atherogenic than the larger, lighter particles, based on the experimental findings that smaller LDL particles are more susceptible for oxidation in vitro, have lower binding affinity for the LDL receptors and lower catabolic rate, have a higher concentration of polyunsaturated fatty acids, and potentially interact more easily with proteoglycans of the arterial wall. Clinical studies have shown that a smaller LDL subfraction profile is associated with an increased risk of heart disease, even when total cholesterol level is only slightly raised. There is a strong inverse association between LDL particle size and triglyceride concentrations. Although LDL particle size is genetically determined, its phenotypic expression may also be affected by environmental factors such as drugs, diet, obesity, exercise or disease. Factors that shift the LDL subfractions profile towards larger particles may reduce the risk of heart disease.
10. Evidence type: nested case-control study
Association of Small Low-Density Lipoprotein Particles With the Incidence of Coronary Artery Disease in Men and Women.
Christopher D. Gardner, PhD; Stephen P. Fortmann, MD; Ronald M. Krauss, MD
JAMA. 1996;276(11):875-881. doi:10.1001/jama.1996.03540110029028.
Incident CAD cases were identified through FCP surveillance between 1979 and 1992. Controls were matched by sex, 5-year age groups, survey time point, ethnicity, and FCP treatment condition. The sample included 124 matched pairs: 90 pairs of men and 34 pairs of women.
…
LDL size was smaller among CAD cases than controls (mean ±SD) (26.17±1.00nm vs 26.68±0.90nm;P
11. Evidence type: review
The small, dense LDL phenotype and the risk of coronary heart disease: epidemiology, patho-physiology and therapeutic aspects. Lamarche B, Lemieux I, Després JP. Diabetes Metab. 1999 Sep;25(3):199-211.
More than decade ago, several cross-sectional studies have reported differences in LDL particle size, density and composition between coronary heart disease (CHD) patients and healthy controls. Three recent prospective, nested case-control studies have since confirmed that the presence of small, dense LDL particles was associated with more than a three-fold increase in the risk of CHD. The small, dense LDL phenotype rarely occurs as an isolated disorder. It is most frequently accompanied by hypertriglyceridemia, reduced HDL cholesterol levels, abdominal obesity, insulin resistance and by a series of other metabolic alterations predictive of an impaired endothelial function and increased susceptibility to thrombosis.
12. Evidence type: prospective
A prospective, population-based study of low density lipoprotein particle size as a risk factor for ischemic heart disease in men. Lamarche B, St-Pierre AC, Ruel IL, Cantin B, Dagenais GR, Després JP. Can J Cardiol. 2001 Aug;17(8):859-65.
Analyses were conducted in a cohort of 2057 men who were all initially free of IHD, and who were followed up over a five-year period, during which 108 first IHD events (myocardial infarction, angina or coronary death) were recorded. LDL particle size was measured by nondenaturing gradient gel electrophoresis.
RESULTS: Cox proportional hazards analysis indicated that the relationship between LDL particle size and the risk of future IHD events was not linear. Men with an LDL particle size less than 256.0 A had a significant 2.2-fold increase in the five-year rate of IHD (P<0.001) compared with men having an LDL particle size greater than 256.0 A. Multivariate and subgroup analyses indicated that small, dense LDL particles predicted the rate of IHD independent of LDL cholesterol, triglycerides, high density lipoprotein (HDL) cholesterol, apolipoprotein B and the total cholesterol to HDL cholesterol ratio. Finally, the magnitude of the increase in IHD risk attributed to lipid risk factors was modulated to a significant extent by variations in LDL particle size.
13. Evidence type: review
Small, dense low-density-lipoproteins and the metabolic syndrome. Rizzo M, Berneis K. Diabetes Metab Res Rev. 2007 Jan;23(1):14-20.
Small, dense low-density-lipoproteins (LDL) are associated with increased risk for cardiovascular diseases and diabetes mellitus and a reduction in LDL size has been reported in patients with coronary and non-coronary forms of atherosclerosis. LDL size has been accepted as an important predictor of cardiovascular events and progression of coronary artery disease as well as an emerging cardiovascular risk factor by the National Cholesterol Education Program Adult Treatment Panel III. Small, dense LDL, with elevated triglyceride levels and low HDL-cholesterol concentrations, constitute the 'atherogenic lipoprotein phenotype (ALP)', a form of atherogenic dyslipidemia that is a feature of type 2 diabetes and the metabolic syndrome.
14. Evidence type: meta-analysis of prospective studies
Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Prospective Studies Collaboration, Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, Qizilbash N, Peto R, Collins R. Lancet. 2007 Dec 1;370(9602):1829-39.
Of various simple indices involving HDL cholesterol, the ratio total/HDL cholesterol was the strongest predictor of IHD mortality (40% more informative than non-HDL cholesterol and more than twice as informative as total cholesterol). Total cholesterol was weakly positively related to ischaemic and total stroke mortality in early middle age (40-59 years), but this finding could be largely or wholly accounted for by the association of cholesterol with blood pressure. Moreover, a positive relation was seen only in middle age and only in those with below-average blood pressure; at older ages (70-89 years) and, particularly, for those with systolic blood pressure over about 145 mm Hg, total cholesterol was negatively related to haemorrhagic and total stroke mortality.
15. Evidence type: post-hoc analysis
Low Levels of High Density Lipoprotein Cholesterol and Increased Risk of Cardiovascular Events in Stable Ischemic Heart Disease Patients: A Post Hoc Analysis from the COURAGE Trial. Acharjee S, Boden WE, Hartigan PM, Teo KK, Maron DJ, Sedlis SP, Kostuk W, Spertus JA, Dada M, Chaitman BR, Mancini GB, Weintraub WS. J Am Coll Cardiol. 2013 Aug 8. pii: S0735-1097(13)03082-9. doi: 10.1016/j.jacc.2013.07.051. [Epub ahead of print]
Abstract:
OBJECTIVES: The aim of this study was to assess the independent effect of high-density lipoprotein cholesterol (HDL-C) level on cardiovascular risk in patients with stable ischemic heart disease (SIHD) while on optimal medical therapy (OMT).BACKGROUND: While low HDL-C level is a powerful and independent predictor of cardiovascular risk, recent data suggest that this may not apply when low-density lipoprotein cholesterol (LDL-C) is reduced to optimal levels using intensive statin therapy.
METHODS: We performed a post hoc analysis in 2,193 men and women with stable ischemic heart disease (SIHD) from the COURAGE trial. The primary outcome measure was the composite of death from any cause or nonfatal myocardial infarction (MI). The independent association between HDL-C levels measured after 6 months on optimal medical therapy (OMT) and the rate of cardiovascular events after 4 years was assessed. Similar analyses were performed separately in subjects with LDL-C levels below 70 mg/dL (1.8 mmol/L).
RESULTS: In the overall population, the rate of death/MI was 33% lower in the highest HDL-C quartile as compared with the lowest quartile, with quartile of HDL-C being a significant, independent predictor of death/MI (P = 0.05), but with no interaction for LDL-C category (P=0.40). Among subjects with LDL-C levels < 70 mg/dL, those in the highest quintile of HDL-C had a 65% relative risk reduction in death or MI as compared to the lowest quintile, with HDL-C quintile demonstrating a significant, inverse predictive effect (P=0.02).
CONCLUSIONS: In this post hoc analysis, patients with SIHD continued to experience incremental cardiovascular risk associated with low HDL-C levels despite OMT during long-term follow-up. This relationship persisted and appeared more prominent even when LDL-C was reduced to optimal levels with intensive dyslipidemic therapy.
16. Evidence type: meta-analysis of prospective studies
Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. Hokanson JE, Austin MA. J Cardiovasc Risk. 1996 Apr;3(2):213-9.
Seventeen studies were selected for the analysis based on published reports of population-based, prospective studies, including 46413 men and 10864 women. To insure comparability, only studies reporting the association between fasting triglyceride levels and incident cardiovascular endpoints were included. Using standard meta-analysis calculations, relative risks (RR) and 95% confidence intervals (CI) were calculated and standardized with respect to a 1 mmol/l increase in triglyceride. Multivariable-adjusted RRs were determined for the six studies in men and two studies in women that reported adjustments for HDL cholesterol.
RESULTS: For men and women, the univariate RRs for triglyceride were 1.32 (95% Cl 1.26-1.39) and 1.76 (95% Cl 1.50-2.07), respectively, indicating an approximately 30% increased risk in men and a 75% increase in women. Adjustment of HDL cholesterol and other risk factors attenuated these RRs to 1.14 (95% Cl 1.05-1.28) and 1.37 (95% Cl 1.13-1.66), respectively, which were still statistically significant values.CONCLUSION: Based on combined data from prospective studies, triglyceride is a risk factor for cardiovascular disease for both men and women in the general population, independent of HDL cholesterol. These finding demonstrate the necessity for clinical trials to evaluate whether lowering plasma triglyceride decreases the risk of cardiovascular disease.
17. Evidence type: prospective cohort study
A prospective study of triglyceride level, low-density lipoprotein particle diameter, and risk of myocardial infarction. Stampfer MJ, Krauss RM, Ma J, Blanche PJ, Holl LG, Sacks FM, Hennekens CH. JAMA. 1996 Sep 18;276(11):882-8.
RESULTS: Cases (n=266) had a significantly smaller LDL diameter (mean [SD], 25.6 [0.9] nm) than did controls (n=308) matched on age and smoking (mean [SD], 25.9 [8] nm; P<.001). Cases also had higher median triglyceride levels (1.90 vs 1.49 mmol/L [168 vs 132 mg/dL]; P<.001). The LDL diameter had a high inverse correlation with triglyceride level (r=-0.71), and a high direct correlation with high-density lipoprotein cholesterol (HDL-C) level (r=0.60). We observed a significant multiplicative interaction between triglyceride and total cholesterol (TC) levels (P=.01). After simultaneous adjustment for lipids and a variety of coronary risk factors, LDL particle diameter was no longer a statistically significant risk indicator, with a relative risk (RR) of 1.09 (95% confidence interval [CI], 0.85-1.40) per 0.8-nm decrease. However, triglyceride level remained significant with an RR of 1.40 (95% CI, 1.10-1.77) per 1.13 mmol/L (100-mg/dL) increase. The association between triglyceride level and MI risk appeared linear across the distribution; men in the highest quintile had a risk about 2.5 times that of those in the lowest quintile. The TC level, but not HDL-C level, also remained significant, with an RR of 1.80 (95% CI, 1.44-2.26) per 1.03-mmol/L (40-mg/dL) increase.
CONCLUSIONS: These findings indicate that nonfasting triglyceride levels appear to be a strong and independent predictor of future risk of MI, particularly when the total cholesterol level is also elevated. In contrast, LDL particle diameter is associated with risk of MI, but not after adjustment for triglyceride level. Increased triglyceride level, small LDL particle diameter, and decreased HDL-C levels appear to reflect underlying metabolic perturbations with adverse consequences for risk of MI; elevated triglyceride levels may help identify high-risk individuals.
18. Evidence type: prospective study
The emergence of triglycerides as a significant independent risk factor in coronary artery disease. Assmann G, Schulte H, Funke H, von Eckardstein A. Eur Heart J. 1998 Oct;19 Suppl M:M8-14.
The Prospective Cardiovascular Münster (PROCAM) study involved 4849 middle-aged men who were followed up for 8 years to record the incidence of coronary heart disease (CHD) events according to the risk factors present at study entry. The study showed that fasting levels of triglycerides were an independent risk factor for CHD events, irrespective of serum levels of high density lipoprotein cholesterol (HDL-C) or low density lipoprotein cholesterol (LDL-C). Other independent predictors of CHD included serum levels of LDL-C and HDL-C, age, systolic blood pressure, cigarette smoking, diabetes mellitus, a family history of myocardial infarction and angina pectoris, but did not include total serum cholesterol levels. Individuals with an LDL-C/HDL-C ratio > 5 had a 19.2% chance of experiencing a CHD event in the next 8 years. Furthermore, if an LDL-C/HDL-C ratio > 5 was combined with hypertriglyceridaemia (> or = 2.3 mmol. l-1), the risk of CHD increased to 26.9%. The association between hypertriglyceridaemia and CHD events may be related to the presence of atherogenic, triglyceride-rich particles in plasma, such as LDL and very low density lipoproteins. High triglyceride levels may also predispose to thrombosis.
19. Evidence type: observation
The role of triglycerides in cardiovascular risk. Gandotra P, Miller M. Curr Cardiol Rep. 2008 Nov;10(6):505-11.
Triglycerides' role in coronary heart disease (CHD) risk assessment has long been debated. Although meta-analyses have suggested that triglycerides are an independent risk factor for CHD, a consensus has emerged that triglycerides more appropriately represent a biomarker of CHD risk rather than an independent risk factor. Ongoing studies will determine whether triglyceride lowering confers additional CHD benefit beyond that attained via low-density lipoprotein (LDL) cholesterol reduction. The American Diabetes Association presently recommends lowering elevated triglycerides as a secondary therapeutic target after LDL cholesterol, whereas other organizations, such as the National Cholesterol Education Program, recommend non-high-density lipoprotein cholesterol as the second priority after attaining the LDL cholesterol goal. However, reducing very high triglycerides (ie, > 500 mg/dL) remains a sufficiently high priority in affected individuals.
20. Evidence type: analysis of observational results from a randomized controlled trial
The Triglyceride Issue Revisited: Findings From the Helsinki Heart Study Leena Tenkanen, PhD; Kati Pietilä; Vesa Manninen, MD; Matti Mänttäri, MD Arch Intern Med. 1994;154(23):2714-2720. doi:10.1001/archinte.1994.00420230107012.
Results: Triglycerides occupied a central role in the pattern of associations of the factors studied; in particular, the associations with HDL-C level, blood pressure, and blood glucose level were without threshold values. The prevalence of high triglyceride level plus low HDL-C level was strongly associated with blood pressure and blood glucose level, while the prevalence of low HDL-C level alone was not. Only the subgroup with both high triglyceride and low HDL-C levels showed a substantial CHD risk, while those with low HDL-C levels alone or high triglyceride levels alone showed a marginal risk.
Conclusions: Our results suggest that triglycerides play a central mediating role in the occurrence of several CHD risk factors, especially those related to the insulin resistance syndrome. Because of these interdependencies, the question of an independent effect of triglycerides is not relevant, and when assessing CHD risk, triglycerides should be considered jointly with HDL-C
21. Evidence type: prospective analysis
Relation of High TG–Low HDL Cholesterol and LDL Cholesterol to the Incidence of Ischemic Heart Disease: An 8-Year Follow-up in the Copenhagen Male Study. Jørgen Jeppesen, Hans Ole Hein, Poul Suadicani, Finn Gyntelberg. Arteriosclerosis, Thrombosis, and Vascular Biology. 1997; 17: 1114-1120
High triglyceride (TG) and low HDL cholesterol (HDL-C) is the characteristic dyslipidemia seen in insulin-resistant subjects. We examined the role of this dyslipidemia as a risk factor of ischemic heart disease (IHD) compared with that of high LDL cholesterol (LDL-C) in the Copenhagen Male Study. In total 2910 white men, aged 53 to 74 years, free of cardiovascular disease at baseline, were subdivided into four groups on the basis of fasting concentrations of serum TG, HDL-C, and LDL-C. “High TG–low HDL-C” was defined as belonging to both the highest third of TG and the lowest third of HDL-C; this group encompassed one fifth of the population. “High LDL-C” was defined as belonging to the highest fifth of LDL-C. A control group was defined as not belonging to either of these two groups. “Combined dyslipidemia” was defined as belonging to both dyslipidemic groups. Age-adjusted incidence of IHD during 8 years of follow-up was 11.4% in high TG–low HDL-C, 8.2% in high LDL-C, 6.6% in the control group, and 17.5% in combined dyslipidemia.
...At both low and high levels of total cholesterol and LDL-C, the presence of high TG–low HDL-C approximately doubled the risk of IHD, and individuals with high TG–low HDL-C in the lowest fifth of LDL-C (≤3.6 mmol/L) had a similar risk of IHD to subjects without high TG–low HDL-C in the highest fifth of LDL-C (≥5.3 mmol/L). High TG–low HDL-C thus clearly identified a group at high risk of IHD, though they had LDL-C levels considered to be safe or borderline (<3.4 mmol/L).
22. Evidence type: observational
Fasting Triglycerides, High-Density Lipoprotein, and Risk of Myocardial Infarction. J. Michael Gaziano, MD, MPH; Charles H. Hennekens, MD, DrPH; Christopher J. O’Donnell, MD, MPH; Jan L. Breslow, MD; Julie E. Buring, ScD. Circulation. 1997; 96: 2520-2525 doi: 10.1161/01.CIR.96.8.2520
We examined the interrelationships of fasting triglycerides, other lipid parameters, and nonlipid risk factors with risk of myocardial infarction among 340 cases and an equal number of age-, sex-, and community-matched control subjects. Cases were men or women of <76 years of age with no prior history of coronary disease who were discharged from one of six Boston area hospitals with the diagnosis of a confirmed myocardial infarction. In crude analyses, we observed a significant association of elevated fasting triglycerides with risk of myocardial infarction (relative risk [RR] in the highest compared with the lowest quartile=6.8; 95% confidence interval [CI]=3.8 to 12.1; P for trend <.001). Results were not materially altered after control for nonlipid coronary risk factors. As expected, the relationship was attenuated after adjustment for HDL but remained statistically significant (RR in the highest quartile=2.7; 95% confidence interval [CI]=1.4 to 5.5; P for trend=.016). Furthermore, the ratio of triglycerides to HDL was a strong predictor of myocardial infarction (RR in the highest compared with the lowest quartile=16.0; 95% CI=7.7 to 33.1; P for trend <.001).
23. Evidence type: observational
High Ratio of Triglycerides to HDL-Cholesterol Predicts Extensive Coronary Disease. Protasio Lemos da Luz, Desiderio Favarato, Jose Rocha Faria-Neto Junior, Pedro Lemos, and Antonio Carlos Palandri Chagas. Clinics. 2008 August; 63(4): 427–432. doi: 10.1590/S1807-59322008000400003 PMCID: PMC2664115
High-risk patients (n = 374) submitted for coronary angiography had their lipid variables measured and coronary disease extent scored by the Friesinger index.
RESULTS: The subjects consisted of 220 males and 154 females, age 57.2 ± 11.1 years, with total cholesterol of 210± 50.3 mg/dL, triglycerides of 173.8 ± 169.8 mg/dL, HDL-cholesterol (HDL-c) of 40.1 ± 12.8 mg/dL, LDL-cholesterol (LDL-c) of 137.3 ± 46.2 mg/dL, TG/HDL-c of 5.1 ± 5.3, and a Friesinger index of 6.6 ± 4.7. The relationship between the extent of coronary disease (dichotomized by a Friesenger index of 5 and lipid levels (normal vs. abnormal) was statistically significant for the following: triglycerides, odds ratio of 2.02 (1.31-3.1; p = 0.0018); HDL-c, odds ratio of 2.21 (1.42-3.43; p = 0.0005); and TG/HDL-c, odds ratio of 2.01(1.30-3.09; p = 0.0018). However, the relationship was not significant between extent of coronary disease and total cholesterol [1.25 (0.82-1.91; p = 0.33)] or LDL-c [1.47 (0.96-2.25; p = 0.0842)]. The chi-square for linear trends for Friesinger > 4 and lipid quartiles was statistically significant for triglycerides (p = 0.0017), HDL-c (p = 0.0001), and TG/HDL-c (p = 0.0018), but not for total cholesterol (p = 0.393) or LDL-c (p = 0.0568). The multivariate analysis by logistic regression OR gave 1.3 ± 0.79 (p = .0001) for TG/HDL-c, 0.779 ± 0.074 (p = .0001) for HDL-c, and 1.234 ± 0.097 (p = 0.03) for LDL. Analysis of receiver operating characteristic curves showed that only TG/HDL-c and HDL-c were useful for detecting extensive coronary disease, with the former more strongly associated with disease.CONCLUSIONS: Although some lipid variables were associated with the extent of coronary disease, the ratio of triglycerides to HDL-cholesterol showed the strongest association with extent.
24. Evidence type: non-randomized experiment
A Ketogenic Diet Favorably Affects Serum Biomarkers for Cardiovascular Disease in Normal-Weight Men. Matthew J. Sharman, William J. Kraemer, Dawn M. Love, Neva G. Avery, Ana L. Gómez, Timothy P. Scheett, and Jeff S. Volek. J. Nutr. July 1, 2002 vol. 132 no. 7 1879-1885
The primary objective of this study was to examine how healthy normolipidemic, normal-weight men respond to a ketogenic diet in terms of fasting and postprandial CVD biomarkers. Ketogenic diets have been criticized on the grounds they jeopardize health (8); however, very few studies have directly evaluated the effects of a ketogenic diet on fasting and postprandial risk factors for CVD. Subjects consumed a diet that consisted of 8% carbohydrate (<50 g/d), 61% fat, and 30% protein. Adaptation to this ketogenic diet resulted in significant reductions in fasting TAG (−33%), postprandial lipemia after a fat-rich meal (−29%), and fasting insulin concentrations (−34%). There were significant increases in LDL particle size, and no change in the oxidative LDL concentrations. There was a significant increase in HDL cholesterol at wk 3 after the ketogenic diet. Collectively, the responses in serum lipids, insulin and lipid subclasses to the ketogenic diet were favorable in terms of overall CVD risk profile.
25. Evidence type: review of experiments
Cardiovascular and hormonal aspects of very-low-carbohydrate ketogenic diets. Volek JS, Sharman MJ. Obes Res. 2004 Nov;12 Suppl 2:115S-23S.
Compared with low-fat diets, short-term VLCKDs [very low carb diets] consistently result in improvements in fat loss, fasting and postprandial triacylglycerols, high-density lipoprotein-cholesterol, the distribution of low-density lipoprotein-cholesterol subclasses, and insulin resistance.
26. Evidence type: randomized controlled trial
Long-term effects of a ketogenic diet in obese patients. Dashti HM, Mathew TC, Hussein T, Asfar SK, Behbahani A, Khoursheed MA, Al-Sayer HM, Bo-Abbas YY, Al-Zaid NS. Exp Clin Cardiol. 2004 Fall;9(3):200-5.
The level of total cholesterol showed a significant decrease from week 1 to week 24 (Figure 3). The level of HDL cholesterol significantly increased (Figure 4), whereas LDL cholesterol levels significantly decreased with treatment (Figure 5). The level of triglycerides decreased significantly after 24 weeks of treatment. The initial level of triglycerides was 2.75±0.23 mmol/L, whereas at week 24, the level decreased to 1.09±0.08 mmol/L (Figure 6).
27. Evidence type: randomized controlled trial
Very Low-Carbohydrate and Low-Fat Diets Affect Fasting Lipids and Postprandial Lipemia Differently in Overweight Men. Matthew J. Sharman, Ana L. Gómez, William J. Kraemer, and Jeff S. Volek. J. Nutr. April 1, 2004 vol. 134 no. 4 880-885
The primary purpose of this study was to compare the effects of a very low-carbohydrate and a low-fat diet on fasting blood lipids and postprandial lipemia in overweight men. In a balanced, randomized, crossover design, overweight men (n = 15; body fat >25%; BMI, 34 kg/m2) consumed 2 experimental diets for 2 consecutive 6-wk periods. One was a very low-carbohydrate (<10% energy as carbohydrate) diet and the other a low-fat (<30% energy as fat) diet. Blood was drawn from fasting subjects on separate days and an oral fat tolerance test was performed at baseline, after the very low-carbohydrate diet period, and after the low-fat diet period. Both diets had the same effect on serum total cholesterol, serum insulin, and homeostasis model analysis-insulin resistance (HOMA-IR). Neither diet affected serum HDL cholesterol (HDL-C) or oxidized LDL (oxLDL) concentrations. Serum LDL cholesterol (LDL-C) was reduced (P < 0.05) only by the low-fat diet (−18%). Fasting serum triacylglycerol (TAG), the TAG/HDL-C ratio, and glucose were significantly reduced only by the very low-carbohydrate diet (−44, −42, and −6%, respectively). Postprandial lipemia was significantly reduced when the men consumed both diets compared with baseline, but the reduction was significantly greater after intake of the very low-carbohydrate diet. Mean and peak LDL particle size increased only after the very low-carbohydrate diet. The short-term hypoenergetic low-fat diet was more effective at lowering serum LDL-C, but the very low-carbohydrate diet was more effective at improving characteristics of the metabolic syndrome as shown by a decrease in fasting serum TAG, the TAG/HDL-C ratio, postprandial lipemia, serum glucose, an increase in LDL particle size, and also greater weight loss (P < 0.05).
28. Evidence type: uncontrolled trial
Long term effects of ketogenic diet in obese subjects with high cholesterol level. Dashti HM, Al-Zaid NS, Mathew TC, Al-Mousawi M, Talib H, Asfar SK, Behbahani AI. Mol Cell Biochem. 2006 Jun;286(1-2):1-9. Epub 2006 Apr 21.
In this study, 66 healthy obese subjects with body mass index (BMI) greater than 30, having high cholesterol level (Group I; n = 35) and those subjects with normal cholesterol level (Group II; n = 31) were selected. The body weight, body mass index, total cholesterol, LDL-cholesterol, HDL-cholesterol, urea, creatinine, glucose and triglycerides were determined before and after the administration of the ketogenic diet. Changes in these parameters were monitored at 8, 16, 24, 32, 40, 48 and 56 weeks of the treatment.
RESULTS: The body weight and body mass index of both groups decreased significantly (P < 0.0001). The level of total cholesterol, LDL cholesterol, triglycerides and blood glucose level decreased significantly (P < 0.0001), whereas HDL cholesterol increased significantly (P < 0.0001) after the treatment in both groups.
CONCLUSION: This study shows the beneficial effects of ketogenic diet following its long term administration in obese subjects with a high level of total cholesterol. Moreover, this study demonstrates that low carbohydrate diet is safe to use for a longer period of time in obese subjects with a high total cholesterol level and those with normocholesterolemia.
29. Evidence type: randomized controlled trial
Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, Golan R, Fraser D, Bolotin A, Vardi H, Tangi-Rozental O, Zuk-Ramot R, Sarusi B, Brickner D, Schwartz Z, Sheiner E, Marko R, Katorza E, Thiery J, Fiedler GM, Blüher M, Stumvoll M, Stampfer MJ; Dietary Intervention Randomized Controlled Trial (DIRECT) Group. N Engl J Med. 2008 Jul 17;359(3):229-41. doi: 10.1056/NEJMoa0708681.
Changes in lipid profiles during the weight-loss and maintenance phases are shown in Figure 3. HDL cholesterol (Figure 3A) increased during the weight-loss and maintenance phases in all groups, with the greatest increase in the low-carbohydrate group (8.4 mg per deciliter [0.22 mmol per liter], P<0.01 for the interaction between diet group and time), as compared with the low-fat group (6.3 mg per deciliter [0.16 mmol per liter]). Triglyceride levels (Figure 3B) decreased significantly in the low-carbohydrate group (23.7 mg per deciliter [0.27 mmol per liter], P=0.03 for the interaction between diet group and time), as compared with the low-fat group (2.7 mg per deciliter [0.03 mmol per liter]). LDL cholesterol levels (Figure 3C) did not change significantly within groups, and there were no significant differences between the groups in the amount of change. Overall, the ratio of total cholesterol to HDL cholesterol (Figure 3D) decreased during both the weight-loss and the maintenance phases. The low-carbohydrate group had the greatest improvement, with a relative decrease of 20% (P=0.01 for the interaction between diet group and time), as compared with a decrease of 12% in the low-fat group.
30. Evidence type: review
Influence of dietary carbohydrate and fat on LDL and HDL particle distributions. Siri PW, Krauss RM. Curr Atheroscler Rep. 2005 Nov;7(6):455-9.
Variations in the size and density distributions of low-density lipoprotein (LDL) and high-density lipoprotein (HDL) particles have been related to risk for cardiovascular disease. In particular, increased levels of small, dense LDL particles, together with reduced levels of large HDL and increases in small HDL, are integral features of the atherogenic dyslipidemia found in patients with insulin resistance, obesity, and metabolic syndrome. Increased dietary carbohydrates, particularly simple sugars and starches with high glycemic index, can increase levels of small, dense LDL and HDL, primarily by mechanisms that involve increasing plasma triglyceride concentrations. Low-carbohydrate diets may have the opposite effects. Diets with differing fatty acid composition can also influence LDL and HDL particle distributions.
31. Evidence type: controlled experiment
Carbohydrate restriction has a more favorable impact on the metabolic syndrome than a low fat diet. Volek JS, Phinney SD, Forsythe CE, Quann EE, Wood RJ, Puglisi MJ, Kraemer WJ, Bibus DM, Fernandez ML, Feinman RD. Lipids. 2009 Apr;44(4):297-309. doi: 10.1007/s11745-008-3274-2. Epub 2008 Dec 12.
Abstract
We recently proposed that the biological markers improved by carbohydrate restriction were precisely those that define the metabolic syndrome (MetS), and that the common thread was regulation of insulin as a control element. We specifically tested the idea with a 12-week study comparing two hypocaloric diets (approximately 1,500 kcal): a carbohydrate-restricted diet (CRD) (%carbohydrate:fat:protein = 12:59:28) and a low-fat diet (LFD) (56:24:20) in 40 subjects with atherogenic dyslipidemia. Both interventions led to improvements in several metabolic markers, but subjects following the CRD had consistently reduced glucose (-12%) and insulin (-50%) concentrations, insulin sensitivity (-55%), weight loss (-10%), decreased adiposity (-14%), and more favorable triacylglycerol (TAG) (-51%), HDL-C (13%) and total cholesterol/HDL-C ratio (-14%) responses. In addition to these markers for MetS, the CRD subjects showed more favorable responses to alternative indicators of cardiovascular risk: postprandial lipemia (-47%), the Apo B/Apo A-1 ratio (-16%), and LDL particle distribution. Despite a threefold higher intake of dietary saturated fat during the CRD, saturated fatty acids in TAG and cholesteryl ester were significantly decreased, as was palmitoleic acid (16:1n-7), an endogenous marker of lipogenesis, compared to subjects consuming the LFD. Serum retinol binding protein 4 has been linked to insulin-resistant states, and only the CRD decreased this marker (-20%). The findings provide support for unifying the disparate markers of MetS and for the proposed intimate connection with dietary carbohydrate. The results support the use of dietary carbohydrate restriction as an effective approach to improve features of MetS and cardiovascular risk.
32. Evidence type: randomized controlled trial
Effect of a low-carbohydrate, ketogenic diet program compared to a low-fat diet on fasting lipoprotein subclasses. Westman EC, Yancy WS Jr, Olsen MK, Dudley T, Guyton JR. Int J Cardiol. 2006 Jun 16;110(2):212-6. Epub 2005 Nov 16.
Comparing baseline to 6 months, the LCKD [low carb ketogenic diet] group had significant changes in large VLDL (-78%), medium VLDL (-60%), small VLDL (-57%), LDL particle size (+2%), large LDL (+54%), medium LDL (-42%), small LDL (-78%), HDL particle size (+5%), large HDL (+21%), and LDL particle concentration (-11%).
...CONCLUSIONS: The LCKD with nutritional supplementation led to beneficial changes in serum lipid subclasses during weight loss. While the LCKD did not lower total LDL cholesterol, it did result in a shift from small, dense LDL to large, buoyant LDL, which could lower cardiovascular disease risk.
33. Evidence type: longitudinal analysis
Change in LDL particle size is associated with change in plasma triglyceride concentration. McNamara JR, Jenner JL, Li Z, Wilson PW, Schaefer EJ. Arterioscler Thromb. 1992 Nov;12(11):1284-90.
Low density lipoprotein (LDL) particle size is inversely associated with plasma triglyceride concentration in cross-sectional analyses. In the present study, changes in the LDL particle size of 227 participants of the Framingham Offspring Study were analyzed longitudinally by nondenaturing gradient gel electrophoresis at two examinations that were separated by 3-4 years. All subjects had triglyceride concentrations < 400 mg/dl at both exams. Using laser scanning densitometry to assess mean LDL particle size, 56% of samples displayed a change in size: 41% had a one-band size change, 13% had a two-band change, and 2% had a three-band change. These changes in size corresponded to a 15% change in pattern type, based on pattern A and B terminology. There was a significant inverse association between change in LDL size and change in triglyceride (p < 0.0001) and glucose (p < 0.004) concentrations, body weight (p < 0.02), and age (p < 0.03). There was also a significant positive association with change in high density lipoprotein (HDL) cholesterol concentration (p < 0.0001).
34. Evidence type: observational
Ratio of triglycerides to HDL cholesterol is an indicator of LDL particle size in patients with type 2 diabetes and normal HDL cholesterol levels. Boizel R, Benhamou PY, Lardy B, Laporte F, Foulon T, Halimi S. Diabetes Care. 2000 Nov;23(11):1679-85.
LDL size correlated negatively with plasma triglycerides (TGs) (R2 = 0.52) and positively with HDL cholesterol (R2 = 0.14). However, an inverse correlation between the TG-to-HDL cholesterol molar ratio and LDL size was even stronger (R2 = 0.59). The ratio was > 1.33 in 90% of the patients with small LDL particles (95% CI 79.3-100) and 16.5% of those with larger LDL particles. A cutoff point of 1.33 for the TG-to-HDL cholesterol ratio distinguishes between patients having small LDL values better than TG cutoff of 1.70 and 1.45 mmol/l.
CONCLUSIONS: The TG-to-HDL cholesterol ratio may be related to the processes involved in LDL size pathophysiology and relevant with regard to the risk of clinical vascular disease. It may be suitable for the selection of patients needing an earlier and aggressive treatment of lipid abnormalities.
35. Evidence type: observational
Assessment of LDL particle size by triglyceride/HDL-cholesterol ratio in non-diabetic, healthy subjects without prominent hyperlipidemia. Maruyama C, Imamura K, Teramoto T. J Atheroscler Thromb. 2003;10(3):186-91.
Abstract
Small, dense low-density lipoprotein (LDL) is an atherogenic lipoprotein because of its susceptibility to oxidative modification. However, evaluating LDL size requires highly sophisticated techniques. We investigated potentially convenient biochemical parameters for assessing the presence of small, dense LDL. Thirty-nine male subjects, who had been involved in a work-site health promotion program, were recruited. Subjects were divided into two groups: normal LDL size (> 25.5 nm, Normal LDL group) and small LDL (< /= 25.5 nm, Small LDL group). Significant negative correlations were observed between LDL size and both triglyceride (TG) (p <0.001) and remnant-like particle cholesterol concentrations (p < 0.01), while there was a significant positive correlation between LDL size and the high density lipoprotein cholesterol (HDL-C) concentration (p < 0.01). The TG concentration was a negative and the HDL-C concentration a positive independent variable predicting LDL size in multiple regression analysis (p < 0.0001). Seventy-five percent of the Small LDL group had TG/HDL-C ratios higher than 0.9 using mmol/L or 2.0 using mg/dL, while only 25% of the normal LDL group had ratios above the levels (p = 0.0013). A combined parameter, the TG/HDL-C ratio, is beneficial for assessing the presence of small LDL.
36. Evidence type: review of experiments
Low-carbohydrate diet review: shifting the paradigm. Hite AH, Berkowitz VG, Berkowitz K. Nutr Clin Pract. 2011 Jun;26(3):300-8. doi: 10.1177/0884533611405791.
Note that there is an error in the text accompanying this figure (not visible in our image). The data is attributed to a study by Jakobsen et al., but it comes from the study in 31, by Volek et al.
